The latest HPV vaccination guidelines recommend starting at ages 9 to 12, ideally before sexual activity begins, with a 2-dose series for those vaccinated early and a 3-dose schedule for older teens and immunocompromised individuals. Both males and females should receive the vaccine, with catch-up options up to age 26. Updated schedules and expanded access aim to maximize protection and reduce cancer risks. Keep exploring to learn more about how these guidelines can protect you and loved ones.
Key Takeaways
- CDC recommends HPV vaccination for ages 9-26, with some guidance extending to age 45 based on individual risk.
- For those starting vaccination before age 15, a 2-dose schedule is now recommended, spaced 6-12 months apart.
- The 3-dose series remains for individuals aged 15 and older or immunocompromised, with doses at 0, 1-2, and 6 months.
- Vaccination is advised regardless of sexual activity history to prevent HPV-related cancers and genital warts.
- HPV vaccines are considered safe, highly effective, and have a strong safety record with minimal mild side effects.
Overview of Current HPV Vaccination Recommendations

Current HPV vaccination recommendations aim to protect individuals before they are exposed to the virus. The CDC recommends routine vaccination for boys and girls starting at age 11 or 12, but it can begin as early as age 9. The goal is to immunize individuals before they become sexually active, reducing the risk of HPV-related cancers and genital warts later in life. The vaccination series usually involves two or three doses, depending on your age at initial vaccination. For those aged 15 and older, a three-dose series is recommended, while younger individuals often need only two doses. Staying on schedule guarantees maximum protection. The guidelines emphasize vaccination for all eligible age groups, regardless of sexual history, to prevent HPV-related health issues. Vaccine efficacy has been shown to be high when administered according to the recommended schedule.
Age Groups Targeted for Vaccination in 2023

In 2023, the recommended age range for HPV vaccination includes preteens and teens, starting as early as age 9. It’s important to understand the ideal timing for vaccination during adolescence to guarantee maximum protection. Knowing when to vaccinate helps you stay ahead in preventing HPV-related health issues. Proper vaccination timing is essential for optimal immune response and long-term effectiveness.
Recommended Age Range
Have you wondered which age groups are prioritized for HPV vaccination in 2023? The recommended age range focuses mainly on preteens and young adults to maximize protection before potential exposure. Generally, vaccination is advised for ages 9 to 26, with some guidelines extending to age 45 based on individual risk. This approach aims to prevent HPV-related cancers and conditions early on. Consider this table to understand the focus:
| Age Group | Purpose |
|---|---|
| 9-14 years | Initiate vaccination before sexual activity |
| 15-26 years | Catch-up vaccination for unvaccinated individuals |
| 27-45 years | Shared decision-making with healthcare provider |
| 46+ years | Less common, mainly for high-risk groups |
Sticking to these ranges helps guarantee optimal protection and reduces HPV-related health issues effectively. Understanding vaccination guidelines is key to making informed health decisions.
Vaccination Timing for Teens
To guarantee effective protection against HPV, vaccination is ideally administered during the teen years, before most individuals become sexually active. The CDC recommends giving the vaccine to ages 11 or 12, but it can start as early as age 9. For those who missed the early doses, catch-up vaccination is advised up to age 26. The goal is to ensure immunity before potential exposure to the virus. The vaccination series is typically completed with two doses if started before age 15, spaced 6 to 12 months apart. If you’re between 15 and 26, three doses are recommended over six months. Starting vaccination early maximizes protection and helps prevent HPV-related cancers and genital warts later in life. Understanding the importance of immunization schedules can improve adherence and ensure optimal protection.
Updated Dosage Schedules and Timing
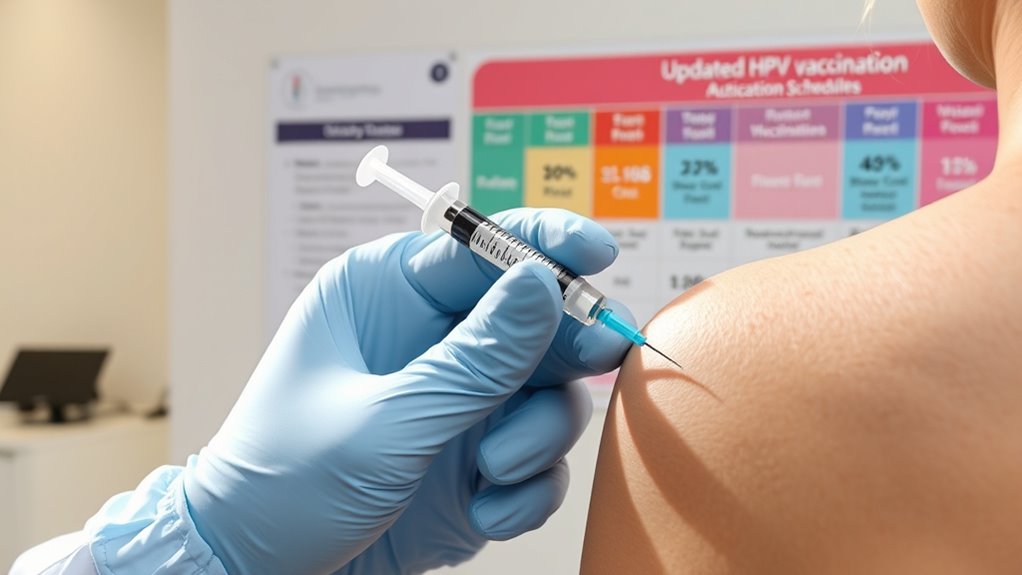
Are you aware of the latest updates to HPV vaccination schedules? The CDC now recommends a two-dose schedule for individuals who start the vaccine series before age 15. You should receive the second dose 6 to 12 months after the first. If you begin the series at age 15 or older, or if you’re immunocompromised, a three-dose schedule applies. The second dose is given 1 to 2 months after the first, and the third dose 6 months after the initial shot. These updates aim to simplify vaccination protocols while maintaining effectiveness. Water parks often feature seasonal events and activities to engage guests. Be sure to follow these timing guidelines to guarantee maximum protection. Staying current with the recommended schedules helps maximize your immunity against HPV-related diseases.
Who Should Receive the HPV Vaccine?

The HPV vaccine is recommended for everyone starting at ages 9 through 26 to protect against HPV-related diseases. If you’re within this age range, getting vaccinated can prevent infections that may lead to cancers or genital warts later in life. It’s most effective when given before any exposure to HPV, which is why early vaccination is vital. For optimal protection, understanding Fokos guidelines and recommendations can help ensure proper vaccination schedules are followed.
Special Considerations for Immunocompromised Individuals

Have you wondered how HPV vaccination guidelines differ for immunocompromised individuals? If you are immunocompromised, such as having HIV, cancer, or taking immunosuppressive therapy, your healthcare provider may recommend a different vaccination schedule. Usually, a three-dose series is advised, but the timing and dosage might be adjusted to maximize protection. These individuals may also have a slightly lower immune response, so completing the full series is especially important. The vaccines are generally safe and well-tolerated, but you should inform your provider about your condition beforehand. It’s essential to follow your healthcare provider’s guidance closely, as they will tailor the vaccination plan to best protect you given your immune status. Additionally, vaccine efficacy may vary in immunocompromised populations, underscoring the importance of adherence to medical advice.
Changes in Vaccination Guidelines for Males and Females
Recent updates to HPV vaccination guidelines have made it easier for both males and females to get protected. The CDC now recommends vaccination starting at age 9, with the preferred age being 11 or 12. For those who haven’t been vaccinated earlier, catch-up doses are advised up to age 26. The guidelines also encourage vaccination for males through age 21 and for men who have sex with men or immunocompromised individuals up to age 26. The vaccination schedule has been simplified, with two doses for those vaccinated before age 15 and three doses for older individuals. These changes aim to improve coverage and prevent HPV-related cancers, making it more accessible and straightforward for you to protect yourself early.
Recommendations for Catch-Up Vaccination

If you missed getting vaccinated earlier, the CDC still recommends catching up on HPV vaccination up to age 26. You should start the series if you’re within this age range, even if you’ve already had some sexual activity, as it can still protect you from HPV-related cancers and conditions. The catch-up schedule varies depending on your age and vaccination history but generally involves two or three doses over several months. If you’re between 15 and 26, you’re eligible for vaccination, regardless of whether you’ve been exposed to HPV. For those with compromised immune systems, the recommendation extends up to age 26. Getting vaccinated now can still provide significant protection, so talk to your healthcare provider about the best plan for you. Additionally, understanding the reviews of different vaccination programs can help you make an informed decision.
Addressing Common Concerns and Myths

Many people have concerns about the safety and side effects of the HPV vaccine. You might have heard myths claiming it’s unsafe or ineffective, but the evidence shows it’s thoroughly tested and highly effective. Understanding the facts can help you make confident decisions about vaccination. In addition, staying informed about the latest guidelines ensures you have accurate information to protect your health.
Vaccine Safety Myths
Despite widespread concerns, the HPV vaccine has a strong safety record backed by extensive research and monitoring. Many myths suggest the vaccine causes serious health problems, but studies show otherwise. The CDC and FDA continuously review safety data, confirming that adverse reactions are rare and usually mild, like soreness or dizziness. Some worry that the vaccine can cause infertility or other long-term issues, but no evidence supports these claims. The vaccine undergoes rigorous testing before approval and ongoing surveillance afterward. Additionally, decluttering efforts in health education help dispel misinformation and promote informed decision-making. It’s important to rely on credible sources and scientific evidence rather than rumors or misinformation. Protecting yourself through vaccination is safe and essential for preventing HPV-related cancers, and concerns rooted in myths shouldn’t prevent you from getting protected.
Effectiveness and Side Effects
The HPV vaccine is highly effective at preventing infections that can lead to cancer, providing long-lasting protection when administered as recommended. Most people experience minimal side effects, making it a safe choice. Common side effects include soreness at the injection site, mild fever, or dizziness, which usually resolve quickly. Serious side effects are rare but can include allergic reactions. Some myths suggest the vaccine causes infertility or contains harmful ingredients, but scientific evidence shows these claims are false. The benefits of vaccination far outweigh the minimal risks. Protect yourself from HPV-related cancers by following current guidelines and discussing any concerns with your healthcare provider.
- Effectively prevents most HPV infections
- Side effects are typically mild and temporary
- Serious adverse reactions are extremely rare
- The vaccine does not cause infertility
- Myths about harmful ingredients are unfounded
How to Access the HPV Vaccine and Next Steps

Wondering how to get the HPV vaccine? First, check with your healthcare provider or local health clinic to see if you’re eligible. Many clinics offer the vaccine at no cost or through insurance plans. If you’re a teen or young adult, talk to your doctor about scheduling your doses. For adults, ask about vaccination options and recommendations based on your age and health history. You can also explore community health programs or school-based clinics that provide vaccines. Once you receive your first dose, remember to complete the series on schedule for maximum protection. Keep track of your appointments and follow-up. Staying proactive is the key to safeguarding yourself against HPV-related health problems.
Frequently Asked Questions
Are There Any New HPV Vaccine Options Introduced Recently?
You’re wondering if new HPV vaccine options have been introduced recently. As of October 2023, the main vaccines available are Gardasil 9 and Cervarix. Gardasil 9 covers nine HPV types and is widely recommended. There haven’t been any new vaccines approved or released lately. It’s best to consult your healthcare provider to determine which vaccine suits your needs and stays current with the latest guidelines.
How Effective Is the HPV Vaccine Against Current Strains?
You might wonder how well the HPV vaccine works against current strains. The good news is, it’s highly effective, especially when you get vaccinated before exposure to the virus. The vaccine covers the most common high-risk strains, considerably reducing your chances of developing related cancers or genital warts. While no vaccine offers 100% protection, staying up-to-date with the latest guidelines ensures you’re best protected against the evolving HPV landscape.
Can the HPV Vaccine Be Administered Alongside Other Vaccines?
Think of your immune system as a busy city, where each vaccine is a helpful worker. You can safely give the HPV vaccine alongside other vaccines; they don’t compete or cause trouble. Healthcare providers often administer multiple vaccines during a single visit to keep your defenses strong. Just make sure to follow your doctor’s advice, and you’ll be building a fortress of protection without missing a beat.
What Are the Common Side Effects Reported Post-Vaccination?
After getting the HPV vaccine, you might notice some common side effects. These usually include soreness, redness, or swelling at the injection site. You could also experience mild fever, headache, fatigue, or nausea. These symptoms are normal and tend to go away within a few days. If you notice severe pain, allergic reactions, or persistent symptoms, it’s important to seek medical advice promptly.
Is There Ongoing Research for Broader HPV Strain Coverage?
Did you know that over 200 HPV strains are known, yet current vaccines target only a few? You might wonder if research is ongoing for broader coverage. The answer is yes; scientists are actively developing next-generation vaccines aimed at protecting against more strains. These efforts could considerably reduce HPV-related cancers worldwide. So, yes, ongoing research continues to improve vaccine effectiveness and offer broader protection for everyone.
Conclusion
By following these updated guidelines, you’ll be arming yourself with the most powerful weapon against HPV—like a shield that deflects every virus attack. Getting vaccinated isn’t just a small step; it’s like building an impenetrable fortress around your health, protecting you from future harm. Don’t wait—seize this life-changing opportunity now and stand tall, confidently facing the world, knowing you’ve taken the ultimate action to safeguard your future!