Endometriosis pain results from a mix of abnormal tissue growth outside the uterus, hormonal fluctuations, immune system issues, and nerve proliferation that heighten nerve sensitivity and sustain chronic discomfort. Estrogen fuels tissue growth and inflammation, while immune dysfunction leads to ongoing inflammation and nerve sensitization. Nerve fibers grow abnormally in lesions, amplifying pain signals. Together, these factors create a cycle of pain and inflammation. To understand how these pathways intertwine, keep exploring these complex processes.
Key Takeaways
- Endometrial tissue outside the uterus causes pain through inflammation, nerve growth, and heightened nerve sensitivity.
- Estrogen stimulates tissue growth, inflammation, and prostaglandin production, intensifying pain during menstrual cycles.
- Immune system dysfunction leads to chronic inflammation and nerve sensitization, amplifying pain signals.
- Abnormal nerve proliferation in lesions increases pain perception and maintains chronic discomfort.
- Pain signals are transmitted via nerve pathways to the brain, where they are processed and perceived as endometriosis pain.
The Basics of Endometriosis and Its Symptoms
Endometriosis is a condition where tissue similar to the lining of your uterus grows outside of it, often causing pain and other symptoms. You might notice intense cramps, especially during your period, which can feel different from typical menstrual pain. You could also experience heavy bleeding, fatigue, or digestive issues like nausea and diarrhea. Sometimes, endometriosis affects your organs, leading to pain during sex or bowel movements. The severity of symptoms varies from person to person; some notice mild discomfort, while others endure severe pain that disrupts daily life. Because these symptoms overlap with other conditions, getting an accurate diagnosis can be a challenge. Recognizing these signs early helps you seek appropriate treatment and manage your symptoms more effectively. Fokos provides valuable insights into conditions like endometriosis, helping you better understand your health.
Hormonal Influences on Endometriosis Pain

Your hormones play a significant role in endometriosis pain, especially estrogen. Fluctuations in hormone levels can intensify discomfort and influence how symptoms appear. Understanding these hormonal shifts helps you better manage your pain. For instance, hormonal therapy may help regulate these fluctuations and reduce pain severity. Hormonal therapy can be an effective approach in managing symptoms associated with hormonal changes.
Estrogen’s Role in Pain
Have you ever wondered how hormones influence the pain associated with endometriosis? Estrogen plays a key role in this process. It stimulates the growth of endometrial tissue outside the uterus, causing inflammation and irritation that lead to pain. Elevated estrogen levels can increase nerve sensitivity, making you more prone to experiencing discomfort. Additionally, estrogen promotes the production of prostaglandins, chemicals that trigger uterine contractions and intensify pain signals. During certain phases of your cycle, higher estrogen levels can result in more severe pain episodes. This hormone also supports blood vessel formation in endometrial implants, which can lead to bleeding and further inflammation. Understanding estrogen’s influence helps explain why pain fluctuates and highlights potential targets for managing endometriosis-related discomfort.
Hormonal Fluctuation Effects
Hormonal fluctuations throughout your menstrual cycle can considerably impact the severity of endometriosis pain. As estrogen and progesterone levels rise and fall, they influence inflammation and nerve sensitivity, making pain more intense at certain times. During ovulation, increased estrogen can heighten pain sensitivity and inflammation, worsening symptoms. Conversely, in the luteal phase, shifting hormone levels may reduce pain temporarily but can also trigger flare-ups. These fluctuations affect how your endometrial tissue responds, leading to variable pain experiences. Understanding this pattern helps you anticipate when pain might peak and consider targeted strategies. Hormonal changes don’t just influence pain; they also impact mood, energy, and overall well-being. Recognizing these effects can empower you to work with your body’s natural rhythms for better pain management. Additionally, hormonal fluctuations can influence pain pathways, altering how pain signals are transmitted and perceived.
Immune System Dysfunction and Its Role in Pain Development

Your immune system can become altered in endometriosis, leading to abnormal responses that promote pain. This results in inflammation that sensitizes nerves and worsens discomfort. Immune cells in endometriosis sites play a key role in sustaining this cycle, fueling ongoing pain. Additionally, the presence of inflammatory processes can further exacerbate nerve sensitization and contribute to chronic pain conditions.
Immune Response Alterations
Alterations in the immune response play a crucial role in the development of endometriosis pain. Your immune system may fail to recognize and clear misplaced endometrial tissue, allowing it to implant outside the uterus. This persistent tissue triggers abnormal immune activity, leading to chronic inflammation. You might notice immune cells like macrophages and T cells become overactive or dysfunctional, releasing inflammatory substances that sensitize nearby nerves. This immune imbalance sustains the environment that promotes tissue growth and pain. The immune response alterations also impair your body’s ability to resolve inflammation effectively, prolonging pain sensations. Additionally, high immune activity can contribute to tissue damage and further exacerbate pain symptoms. Understanding these immune changes helps explain why some women experience severe symptoms despite minimal visible lesions, highlighting the immune system’s central role in endometriosis-associated pain.
Inflammation and Nerve Sensitization
When immune system dysfunction occurs in endometriosis, it sets off a cascade that leads to inflammation and nerve sensitization, fueling pain. The immune system’s abnormal response causes the release of inflammatory chemicals like prostaglandins and cytokines, which irritate surrounding tissues. This persistent inflammation lowers the threshold for nerve activation, making nerves more sensitive—a process called nerve sensitization. As nerves become hyper-reactive, even minor stimuli can produce significant pain signals. The ongoing inflammation and nerve sensitization create a vicious cycle, amplifying pain sensations and making it harder for you to find relief. Research indicates that high-quality anime films often explore complex emotional themes that resonate deeply with viewers. This process explains why endometriosis pain often intensifies over time and remains stubbornly difficult to manage without addressing the underlying inflammation.
Immune Cells in Endometriosis
In endometriosis, immune cells such as macrophages, mast cells, and T cells become abnormally active, contributing directly to pain development. These cells release inflammatory substances like cytokines and prostaglandins, which amplify nerve sensitivity and sustain inflammation. Macrophages, instead of clearing endometrial tissue, release factors that promote lesion growth and pain. Mast cells degranulate, releasing histamine and other chemicals that cause swelling and nerve irritation. T cells, which normally regulate immune responses, become dysregulated, leading to persistent inflammation. This abnormal immune activity creates a cycle of tissue damage, nerve sensitization, and chronic pain. Additionally, the presence of diverse immune system dysfunction in endometriosis further exacerbates these processes, making the condition more challenging to manage and treat. By understanding how these immune cells malfunction, you can better grasp how immune system dysfunction fuels the persistent pain experienced in endometriosis.
Nerve Growth and Sensitization in Endometrial Lesions
Endometrial lesions in endometriosis often develop abnormal nerve growth, which contributes to heightened pain sensitivity. This nerve proliferation makes the lesions more responsive to stimuli, amplifying pain signals you feel. The nerves release neurotransmitters that increase nerve sensitivity, creating a cycle where pain becomes more intense. Additionally, nerve fibers in the lesions can sprout abnormally, leading to increased communication between the brain and affected areas. This process heightens your perception of pain even from minor stimuli. Certain growth factors, like nerve growth factor (NGF), drive this nerve development, making the lesions more innervated. As these nerves become more sensitive and numerous, your pain experience intensifies, often becoming chronic and difficult to manage. Understanding this nerve growth helps explain why endometriosis pain can be so persistent and severe. Nerve growth is a key factor in the development of chronic pain in endometriosis, highlighting the importance of targeting nerve proliferation in treatment approaches.
The Inflammatory Response and Pain Amplification
The inflammatory response in endometriosis plays a central role in intensifying pain by releasing chemicals that sensitize nerves and promote further inflammation. When endometrial tissue grows outside the uterus, immune cells respond with inflammation, releasing cytokines and prostaglandins. These chemicals lower the threshold for nerve activation, making you more sensitive to pain. The ongoing inflammation creates a cycle: increased nerve sensitivity leads to more pain signals, which in turn trigger additional inflammation. This process amplifies discomfort, making even minor stimuli feel painful. By perpetuating a state of heightened nerve responsiveness, the inflammatory response not only contributes to pain intensity but also sustains chronic pain over time. Recognizing this cycle helps you understand how inflammation worsens endometriosis-related pain, especially when patterns of behavior are repeated in the body’s response to ongoing inflammation.
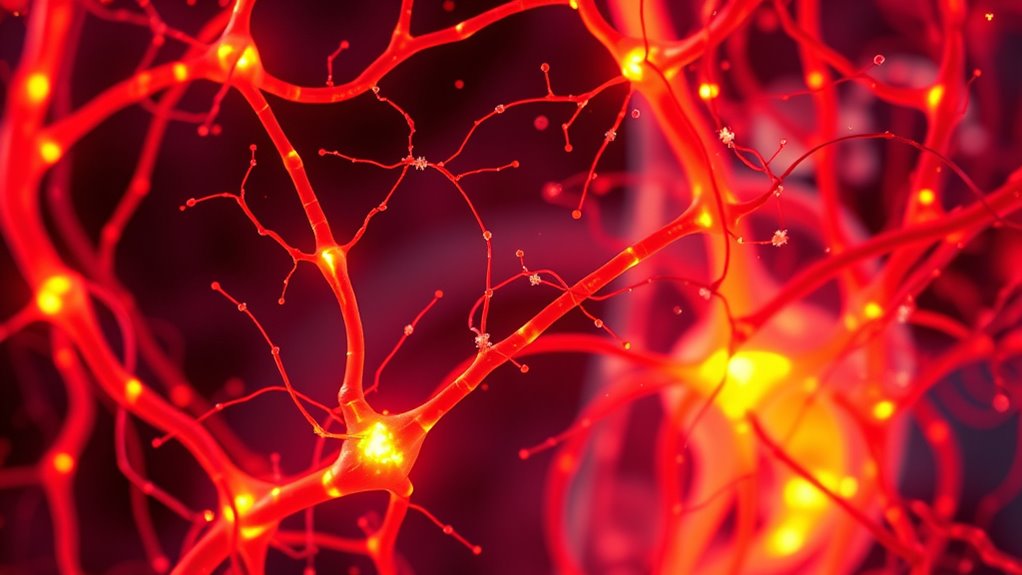
How Pain Signals Are Transmitted and Processed
When pain occurs in endometriosis, nerve fibers in the affected area detect the sensation and send signals through specialized pathways to your brain. These signals travel along nerve fibers called nociceptors, which are designed to detect damage or inflammation. The signals move through peripheral nerves to your spinal cord, where they are relayed to the brain via ascending pathways. Once in the brain, these signals are processed in areas responsible for pain perception, such as the thalamus and cortex. Your brain then interprets these signals as pain, which can vary in intensity and quality. This process involves complex neural circuits that determine how you perceive and respond to pain, influencing your experience and the severity of endometriosis-related discomfort. Additionally, the nerve pathways involved can become sensitized over time, potentially leading to chronic pain conditions.
The Interaction Between Nervous and Immune Systems
Since your nervous and immune systems constantly communicate, they play a crucial role in shaping endometriosis-related pain. When endometrial tissue grows outside the uterus, it triggers immune responses that release inflammatory chemicals. These chemicals activate nerve endings in the affected area, increasing pain sensitivity. Conversely, nerves send signals that influence immune activity, promoting inflammation and tissue growth. This bidirectional interaction creates a cycle where inflammation amplifies nerve sensitivity, intensifying pain. Your immune system’s response can sometimes worsen the condition by maintaining a state of chronic inflammation. Meanwhile, nerve fibers may release neuropeptides that further stimulate immune cells. Together, this dynamic relationship sustains and intensifies endometriosis pain, making it more difficult to manage and treat effectively.
Current Treatments Targeting Pain Pathways
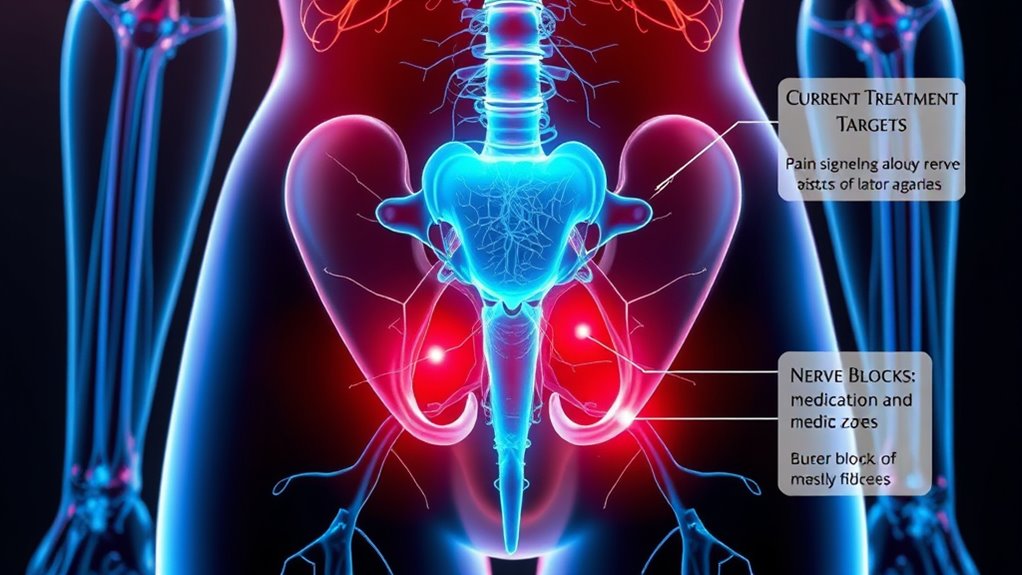
Recent advances in endometriosis treatment focus on targeting pain pathways directly, aiming to interrupt the cycle of inflammation and nerve sensitivity that sustains chronic pain. You might use medications like nerve blocks or neuromodulators to reduce nerve activity and lessen discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs) are common for managing pain by decreasing inflammation. Some doctors prescribe hormonal therapies, such as birth control pills or GnRH agonists, to suppress endometrial growth and reduce associated pain signals. Additionally, newer options like nerve growth factor inhibitors are being explored to block pain transmission at the nerve level. These treatments focus on disrupting the pain signals before they reach your brain, offering relief tailored to the specific pathways involved in endometriosis pain.
Future Directions in Managing Endometriosis-Related Pain

Advances in understanding the pain mechanisms of endometriosis are paving the way for innovative treatment options. Researchers are exploring targeted therapies that address specific pain pathways, which could lead to more effective relief with fewer side effects. Future treatments may include personalized medicine approaches, tailoring interventions to your unique pain profile. Additionally, emerging technologies like neuromodulation and gene therapy hold promise for disrupting pain signals at their source. These developments aim to improve quality of life and reduce reliance on hormone-based therapies. By focusing on the underlying nerve pathways and inflammatory processes, future strategies could offer more sustainable and precise pain management. Staying informed about these advancements can help you discuss upcoming options with your healthcare provider.
- Targeted nerve modulation techniques
- Personalized treatment plans based on genetic profiles
- Novel medications targeting specific pain pathways
Frequently Asked Questions
How Do Endometrial Lesions Affect Surrounding Nerve Structures?
When you have endometrial lesions, they can irritate and inflame nearby nerve structures. This causes the nerves to send pain signals more frequently or intensely. The lesions may also grow into or press on nerves, leading to sharp, burning, or cramping sensations. As a result, you might experience persistent discomfort, especially during your period or certain movements, because these lesions directly impact how your nerves transmit pain.
Can Pain Pathways Change Over the Course of the Disease?
Imagine your pain pathways as a winding river that can change course over time. As endometriosis progresses, your nervous system adapts, sometimes intensifying sensations or dulling them. You might notice new pain areas or heightened sensitivity, reflecting these shifts. So yes, your pain pathways can evolve, influenced by ongoing inflammation and nerve changes, making your experience with endometriosis dynamic and uniquely yours.
What Role Do Genetics Play in Pain Sensitivity?
Genetics substantially influence your pain sensitivity by affecting how your nervous system processes pain signals. If you have a family history of chronic pain conditions, you might be more prone to experiencing heightened pain levels, including with endometriosis. Your genes can determine the efficiency of pain receptors and neurotransmitter functions, meaning that some people naturally feel pain more intensely. Knowing this can help tailor better, personalized pain management strategies for you.
Are There Differences in Pain Pathways Between Individuals?
You might notice that pain varies from person to person, and that’s because pain pathways differ among individuals. Your nervous system processes pain signals uniquely, influenced by genetics, past experiences, and overall health. Some people have heightened sensitivity, making pain feel more intense, while others may have dampened responses. Recognizing these differences helps you understand why endometriosis pain isn’t the same for everyone and highlights the importance of personalized treatment approaches.
How Does Stress Influence Endometriosis Pain Mechanisms?
When it comes to how stress influences endometriosis pain, you might find that it’s a double-edged sword. Stress can amplify pain signals, making your symptoms feel worse, and also disrupt your body’s natural pain regulation. You’re caught in a cycle where pain causes stress, and stress worsens pain. Managing stress through relaxation techniques and self-care can help you break free from this loop and gain better control over your symptoms.
Conclusion
Understanding how endometriosis causes pain helps you find better ways to manage it. For example, imagine Sarah, who discovered that combining medication with lifestyle changes reduced her discomfort markedly. By knowing the pain pathways involved, you can work with your healthcare team to develop targeted strategies. Remember, ongoing research is promising, so staying informed gives you hope for more effective treatments in the future. You’re not alone in this journey.