Even after getting the HPV vaccine, it’s important to continue cervical cancer screening because the vaccine doesn’t protect against all high-risk HPV types. Guidelines recommend starting Pap tests at age 21, with follow-up intervals based on your age and vaccination status. HPV testing is increasingly used alongside Pap tests for better accuracy. To understand why ongoing screening remains essential and how it adapts over time, keep exploring this helpful information.
Key Takeaways
- Vaccinated women should still follow current screening guidelines, starting Pap tests at age 21 and continuing as recommended.
- HPV vaccination reduces risk but does not eliminate the need for regular cervical cancer screening.
- Molecular HPV testing remains effective in vaccinated populations for early detection of high-risk infections.
- Screening intervals may be extended based on age, vaccination status, and test results, per evolving guidelines.
- Patients should be counseled that ongoing screening complements vaccination for optimal cervical health.
Understanding the Impact of HPV Vaccination on Cervical Cancer Risk

HPV vaccination considerably reduces the risk of developing cervical cancer by preventing infection with the most common high-risk HPV types. When you’re vaccinated, your body is better equipped to fight off these virus strains before they cause cellular changes leading to cancer. The vaccine is most effective when administered before exposure to HPV, typically recommended for young adolescents. By reducing the prevalence of high-risk HPV infections in the population, vaccination also lowers the overall risk of cervical cancer. Although vaccination doesn’t eliminate all risk, it markedly decreases your chances of developing the disease later in life. Staying up to date with vaccination offers a powerful protective benefit, especially when combined with regular screenings. This combined approach helps catch any issues early, even if infection occurs. Additionally, ongoing research into vaccine efficacy continues to support its role in cervical cancer prevention.
Current Screening Guidelines for Vaccinated Women

Although vaccination considerably lowers your risk of cervical cancer, it doesn’t eliminate the need for regular screening. Staying vigilant is essential for your health and peace of mind. Current guidelines recommend that you:
- Begin Pap tests at age 21, regardless of vaccination status.
- Have Pap tests every three years if results are normal.
- For women aged 30-65, consider HPV testing combined with Pap every five years.
- Continue screenings until age 65, following your healthcare provider’s advice.
These steps help catch any abnormal changes early, even if you’re vaccinated. Remember, vaccines lower your risk but don’t eliminate it entirely. Regular screenings are your best defense in protecting your future health and preventing cervical cancer.
The Role of HPV Testing in the Post-Vaccination Era

HPV testing plays a vital role in screening, even after vaccination, by accurately identifying high-risk infections. As vaccination rates increase, guidelines are adapting to guarantee testing remains effective and cost-efficient. Understanding how HPV testing fits into post-vaccination screening helps you stay informed about best practices. Incorporating effective screening methods ensures early detection and better management of cervical cancer risks in vaccinated populations.
HPV Testing Effectiveness
As vaccination rates increase, the role of HPV testing in cervical cancer screening has become more nuanced. You might wonder how effective HPV testing remains after widespread vaccination. Here’s what you should know:
- It helps detect high-risk HPV types, reducing missed cases.
- It can identify persistent infections before they develop into cancer.
- Its accuracy remains high, even in vaccinated populations.
- It offers a more sensitive method compared to cytology alone.
- Ongoing research into AI safety measures aims to ensure the reliability of HPV testing technologies in the evolving landscape of cervical cancer prevention.
This means you can trust HPV testing to catch potential problems early, giving you peace of mind. While vaccination reduces risk, HPV testing continues to be a crucial tool in safeguarding your health, especially as the landscape of cervical cancer prevention evolves.
Screening Guidelines Adaptation
With high vaccination coverage reducing the prevalence of high-risk HPV infections, screening guidelines are evolving to reflect the changing landscape. You’ll find that many health authorities now recommend longer intervals between screenings for vaccinated women, since the risk of cervical cancer decreases. HPV testing remains central, often used as the primary screening method, replacing or supplementing Pap smears. For example, women aged 30-65 may be advised to undergo HPV testing every five years instead of every three. These adaptations aim to balance early detection with minimizing unnecessary procedures. You should stay informed about evolving guidelines, as recommendations may differ based on your age, vaccination status, and local healthcare policies. Additionally, understanding screening intervals can help you make more informed health decisions. Ultimately, the goal is to optimize screening efficiency while maintaining protection against cervical cancer.
Age and Timing Considerations for Screening After Vaccination

Deciding when to begin cervical cancer screening after receiving the HPV vaccine depends on your age and vaccination history. Your decisions can impact your health and peace of mind. Consider these key points:
- If you’re under 21, screening usually isn’t recommended, regardless of vaccination.
- For women aged 21-29, Pap tests are advised every 3 years, even if vaccinated.
- Starting at age 30, co-testing with Pap and HPV every 5 years is preferred for vaccinated women.
- If you’re vaccinated later in life, your healthcare provider may adjust screening timing based on your risk.
- Understanding the role of contrast ratio in imaging can help in evaluating the effectiveness of screening methods.
Your vaccination status doesn’t eliminate the need for screening but influences the timing. Talk with your provider to create a plan tailored to your unique situation.
Balancing Screening Frequency With Vaccination Status

Balancing how often you should get screened for cervical cancer depends on both your vaccination status and your overall risk factors. If you’re vaccinated and at low risk, screening intervals may be extended, reducing unnecessary tests. Conversely, unvaccinated or high-risk individuals might need more frequent screenings to catch issues early. Consider this table:
| Vaccination Status | Risk Level | Recommended Screening Interval |
|---|---|---|
| Fully vaccinated | Low | Every 5 years |
| Fully vaccinated | High (e.g., immunocompromised) | Every 3 years |
| Unvaccinated | Low | Every 3-5 years |
| Unvaccinated | High | Every 1-3 years |
Your risk factors influence how you balance screening frequency with vaccination, ensuring ideal protection without overtesting. Additionally, understanding the importance of preventive health measures can help optimize your screening schedule.
Advances in Screening Technologies and Their Relevance

Recent advances in screening technologies are transforming how you detect cervical cancer early. Enhanced detection methods, like more precise cytology, improve accuracy, while molecular testing offers a sensitive way to identify high-risk HPV types. These innovations make your screening process more effective and tailored to individual risk profiles. Additionally, the development of expert tutorials and reviews helps healthcare providers stay informed about the latest techniques and best practices.
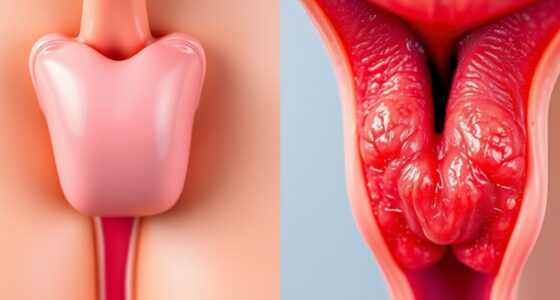
Enhanced Detection Methods
Advances in screening technologies have considerably improved the ability to detect cervical abnormalities early, especially as vaccination changes the landscape of risk. These enhanced methods give you a better chance to catch issues sooner and prevent cancer development. Consider these breakthroughs:
- Liquid-based cytology offers more accurate results and clearer samples, reducing false negatives.
- Automated screening systems increase consistency and help identify abnormal cells more reliably.
- Digital imaging techniques allow for detailed analysis, leading to quicker and more precise diagnoses.
- Enhanced visual inspection tools improve detection of subtle abnormalities, even in challenging cases.
- Staying informed about regional screening guidelines can ensure you are utilizing the most effective detection methods available.
Molecular Testing Advancements
Molecular testing has revolutionized cervical cancer screening by providing highly sensitive and specific methods to detect abnormal cells and HPV infections. These advanced techniques, like HPV DNA and RNA tests, allow you to identify high-risk HPV types more accurately than traditional cytology alone. With molecular testing, you can detect persistent infections that pose a greater risk for progression to cervical cancer. This means fewer false negatives and earlier intervention opportunities. Additionally, molecular tests can be integrated into primary screening programs, streamlining the process and improving efficiency. As a result, you benefit from more precise risk stratification, allowing for tailored follow-up and management. Moreover, the incorporation of specialized testing techniques enhances your ability to differentiate between transient and persistent infections, further refining screening accuracy. Overall, these advancements enhance early detection, reduce unnecessary procedures, and improve outcomes in cervical cancer prevention efforts.
Counseling Patients: Communicating Risks and Recommendations
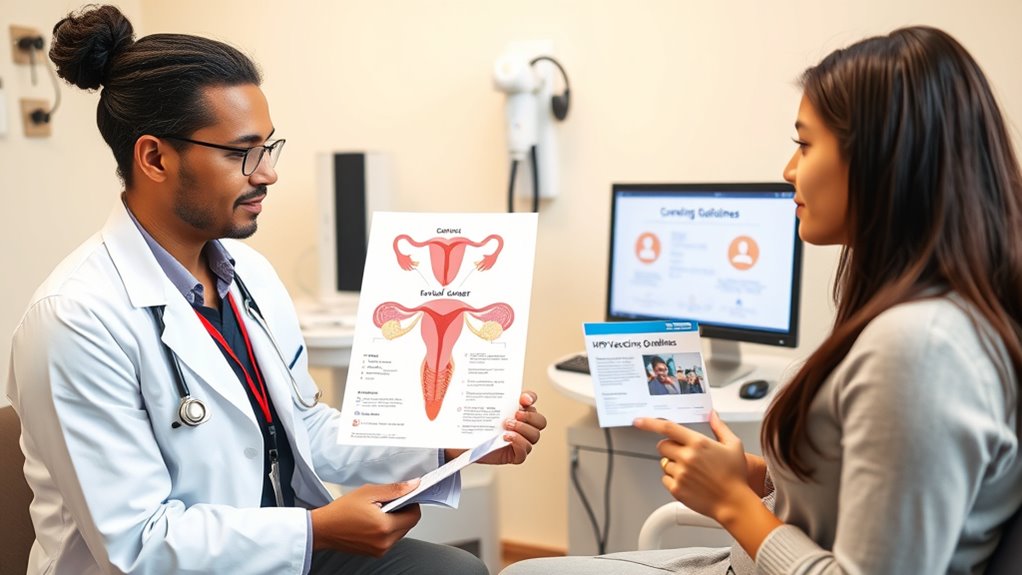
When counseling patients about cervical cancer screening after HPV vaccination, it’s essential to clearly communicate both the ongoing risks and the current recommendations. You need to reassure patients that vaccination doesn’t eliminate the need for screening but reduces their risk. Emphasize that:
Vaccination reduces risk but screening remains essential for cervical health.
- They still face a small chance of developing cervical cancer.
- Screening remains critical for early detection and peace of mind.
- Guidelines may vary based on age and vaccination status.
- Staying informed helps them make empowered health choices.
- Explaining the benefits of Glycolic Acid Exfoliating Toner can help patients understand the importance of ongoing health maintenance alongside skincare.
Use empathetic language to address concerns and clarify misconceptions. Encourage questions and provide tailored advice. Your goal is to foster trust, ensuring patients understand that vaccination is a protective step, but regular screening remains indispensable for their long-term health and safety.
Future Directions in Cervical Cancer Prevention and Screening

As research continues to improve our understanding of HPV and cervical cancer, new strategies are emerging to enhance prevention and screening efforts. You might see advancements like personalized screening schedules based on risk factors, integrating HPV genotyping, and improved biomarkers for early detection. These developments aim to reduce unnecessary procedures while catching cancers early. Additionally, innovative technologies like self-sampling and artificial intelligence are gaining traction, making screening more accessible and accurate. Here’s a snapshot of future directions:
| Strategy | Benefit | Implementation |
|---|---|---|
| Risk-based screening | Tailored, efficient exams | Personalized patient assessment |
| HPV genotyping | Better risk stratification | Advanced laboratory testing |
| Self-sampling | Increased screening uptake | Home collection kits |
| AI diagnostic tools | Faster, accurate detection | Machine learning in labs |
Frequently Asked Questions
How Does the HPV Vaccine Affect the Accuracy of Pap Smears?
You might wonder if the HPV vaccine impacts Pap smear accuracy. The vaccine protects against certain high-risk HPV types that cause most cervical cancers, but it doesn’t eliminate all risks. Consequently, Pap smears remain essential for detecting abnormal cells regardless of vaccination. The vaccine may slightly reduce the number of abnormal results, but it doesn’t replace or diminish the importance of regular screening to catch other potential issues.
Are There Any New Screening Methods Recommended for Vaccinated Women?
Think of cervical cancer screening as your shield, and new methods are like upgraded armor. For vaccinated women, traditional Pap smears remain the gold standard, but HPV DNA testing is increasingly advised as a primary screening tool. You’ll want to stay informed with your healthcare provider about these updates, as they help catch potential issues early. This layered approach ensures you’re protected, regardless of whether you’ve received the HPV vaccine.
When Should Vaccinated Women Start Cervical Cancer Screening?
You should start cervical cancer screening at age 21, regardless of HPV vaccination status. The vaccines don’t protect against all cancer-causing HPV types, so screening remains essential. If you’re vaccinated, you still need Pap tests or co-testing with HPV every three to five years, depending on your age and health history. Regular screening helps detect abnormalities early, ensuring timely treatment and continued health.
Does Vaccination Eliminate the Need for Cervical Cancer Screening Entirely?
You still need to get screened for cervical cancer even if you’re vaccinated. The HPV vaccine doesn’t protect against all cancer-causing HPV types, so screening remains essential. Regular Pap tests and HPV tests help catch any abnormalities early. Vaccination greatly reduces your risk, but it doesn’t eliminate it completely. So, follow your healthcare provider’s screening recommendations to stay protected and catch issues early.
How Do Screening Intervals Differ for Women With Different Vaccination Statuses?
Think of your cervix as a garden that needs regular tending. If you’re vaccinated, your screening intervals might stretch out like a well-maintained walkway, typically every 5 years with co-testing. Unvaccinated women, however, should visit more frequently, around every 3 years. Your vaccination status shapes your screening schedule, helping protect your health and keep your cervical garden flourishing. Always check with your healthcare provider for personalized advice.
Conclusion
As you navigate cervical cancer screening after HPV vaccination, remember that staying informed is key. While vaccination reduces your risk, it’s not a free pass—regular screenings remain essential. Keep the conversation open with your healthcare provider and don’t put all your eggs in one basket. Staying proactive now can make all the difference, so don’t let the grass grow under your feet—your health depends on it.