Psoriasis involves overactive immune pathways where cytokines like IL-17, IL-23, and TNF-alpha promote skin cell growth and inflammation. Dendritic cells trigger these cytokines, activating T cells, especially Th17 cells, which amplify the process. New therapies focus on targeting these cytokines and immune cells with biologics and small molecules, offering more personalized and effective options. Staying informed about these advances helps you understand how emerging treatments may improve your condition.
Key Takeaways
- Psoriasis involves overactive immune responses, particularly Th17 and Th1 cells, releasing cytokines like IL-17, IL-23, and TNF-alpha.
- Dendritic cells initiate inflammation by activating T cells and secreting cytokines that promote immune cell recruitment.
- New therapies target specific cytokines and immune receptors, including biologics against IL-17 and IL-23, and small molecule inhibitors.
- Personalized treatments use biomarkers and genetic profiling to optimize therapy effectiveness and monitor disease activity.
- Ongoing research focuses on discovering novel immune pathways, biomarkers, and innovative drug delivery systems for improved management.
Understanding the Immune System’s Role in Psoriasis
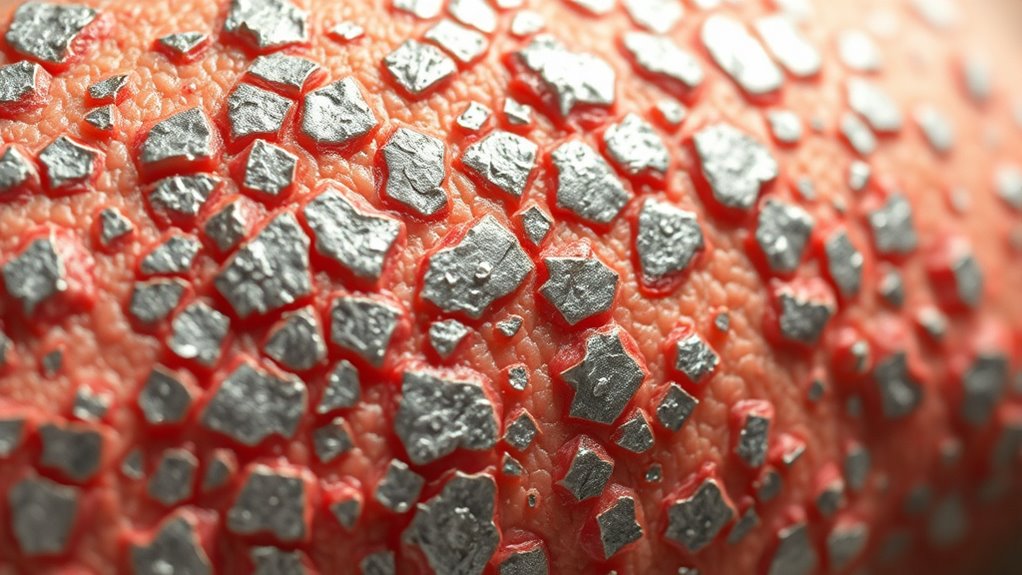
Understanding the immune system’s role in psoriasis is essential because this chronic skin condition results from an overactive immune response. Your immune system mistakenly identifies healthy skin cells as threats, triggering an inflammatory process. This response leads to the rapid growth of skin cells, causing the thick, scaly patches characteristic of psoriasis. When your immune cells, especially T cells, become hyperactive, they release inflammatory signals that amplify the process. This immune activity not only affects the skin but can also involve systemic inflammation. Recognizing this overactivity helps explain why treatments targeting immune pathways are effective. By modulating your immune response, these therapies can reduce symptoms and improve skin health, highlighting the central role your immune system plays in psoriasis development and management.
Key Cytokines Involved in Psoriasis Pathogenesis

Several specific cytokines drive the inflammation and skin changes seen in psoriasis, making them essential to the disease’s development. These signaling proteins promote keratinocyte proliferation, immune cell recruitment, and chronic inflammation. Among the key cytokines are IL-17, IL-23, TNF-alpha, and IFN-gamma. They work together in a complex network, amplifying the immune response and sustaining skin lesions. Recognizing these cytokines helps in targeting therapies effectively. For example, blocking IL-17 or IL-23 can markedly reduce symptoms. It’s important to understand that:
- IL-17 plays a vital role in neutrophil recruitment and keratinocyte activation.
- IL-23 supports Th17 cell differentiation, fueling inflammation.
- TNF-alpha is a master regulator of inflammatory processes.
- These cytokines create a feedback loop that perpetuates psoriasis symptoms.
The Th17 Cell Pathway and Its Impact on Skin Inflammation

The Th17 cell pathway plays a central role in driving skin inflammation in psoriasis by producing cytokines that amplify immune responses. When Th17 cells activate, they release IL-17A, IL-17F, and IL-22, which promote keratinocyte proliferation and attract other inflammatory cells. This cascade results in the thickened, scaly plaques characteristic of psoriasis. You’ll find that IL-17 cytokines stimulate skin cells to produce additional pro-inflammatory molecules, perpetuating the cycle of inflammation. Th17 cells are mainly driven by signals from other immune cells, especially in response to microbial triggers or skin injury. Targeting this pathway has become a key strategy in developing therapies that effectively reduce inflammation and improve symptoms, offering hope for better management of psoriasis. Understanding immune signaling is crucial for advancing targeted treatments in inflammatory skin diseases.
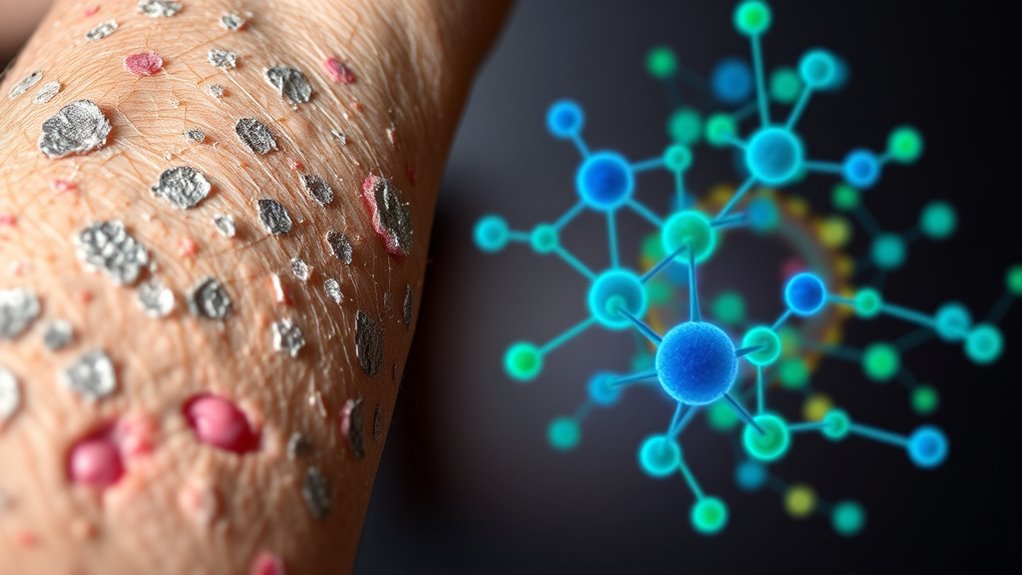
The Influence of Dendritic Cells in Psoriasis Development

Dendritic cells act as the immune system’s sentinels, playing a pivotal role in initiating the inflammatory response in psoriasis. When triggered by environmental factors or skin injury, these cells activate T cells and release cytokines that fuel inflammation. Their key function is processing and presenting antigens, which alert other immune cells to potential threats. In psoriasis, dendritic cells become hyperactive, producing excessive cytokines like TNF-alpha, IL-23, and IL-12. These cytokines promote the activation of Th17 and Th1 cells, amplifying inflammation and keratinocyte proliferation. Additionally, emerging therapies are focusing on dendritic cell pathways to modulate immune responses more precisely.
Genetic Factors and Immune Dysregulation
Genetic factors considerably influence the development and severity of psoriasis by disrupting normal immune regulation. You inherit specific gene variants that affect immune system responses, making you more susceptible. For example, variations in the HLA-C gene are strongly linked to psoriasis risk, influencing how your immune cells recognize skin cells. These genetic predispositions can lead to an overactive immune response, causing your body to mistakenly attack healthy skin tissue. Additionally, other genes involved in cytokine production and immune signaling pathways contribute to immune dysregulation. Understanding your genetic background helps explain why psoriasis varies in severity and presentation among individuals. Genetic predispositions can also interact with environmental triggers, often activating these genetic vulnerabilities, leading to the immune system’s abnormal activation seen in psoriasis.
Traditional Treatments and Their Limitations
You may find that topical remedies provide only temporary relief and often fail to control widespread or severe psoriasis. Systemic therapies can be effective but come with challenges like side effects and variable responses. These limitations highlight the need for more targeted and sustainable treatment options. Incorporating novel therapeutic approaches could potentially improve outcomes and reduce adverse effects.
Topical Remedies Limitations
While topical treatments are often the first line of defense against psoriasis, they come with notable limitations. These remedies may provide relief, but they rarely offer a long-term solution. You might find yourself applying creams or ointments frequently, yet still experiencing flare-ups. Their effectiveness can diminish over time, especially with persistent use. Additionally, some treatments can cause skin irritation or thinning, which limits their suitability for ongoing management. Furthermore, the topical delivery of medication often fails to reach deeper skin layers where inflammation occurs, reducing overall efficacy. Because of these issues, topical remedies often serve only as part of a broader treatment plan rather than a complete solution.
Systemic Therapies Challenges
Systemic therapies are often employed when topical treatments fall short, but they come with their own set of challenges. These treatments can cause significant side effects, such as increased infection risk, liver issues, or blood abnormalities. They also require regular monitoring and can be costly, limiting accessibility. Additionally, some therapies lose effectiveness over time, leading to treatment resistance. You may experience variable responses, making it hard to predict outcomes. Here’s a quick overview:
| Challenge | Impact |
|---|---|
| Side effects | Health risks and need for ongoing monitoring |
| Cost | Financial burden on patients |
| Resistance | Reduced long-term effectiveness |
| Variable response | Unpredictable treatment outcomes |
| Monitoring requirements | Increased healthcare visits and tests |
Furthermore, the immune pathways involved in psoriasis are complex, and targeting them effectively remains a challenge for new therapies.
Biologic Therapies Targeting Cytokines

Biologic therapies targeting cytokines have revolutionized psoriasis treatment by directly interfering with key inflammatory mediators. These therapies specifically block cytokines like TNF-alpha, IL-17, and IL-23, which drive the inflammatory process in psoriasis. By targeting these molecules, you can experience significant skin clearance and symptom relief. Biologics offer a targeted approach with often fewer side effects compared to traditional systemic treatments. They are administered via injections or infusions and require monitoring for infections. AI safety measures are essential to ensure the responsible development and deployment of these advanced therapies.
Emerging Therapies and Future Directions

Emerging therapies in psoriasis focus on novel biologic agents and small molecule inhibitors that target different immune pathways. These options promise more effective and personalized treatments tailored to individual patient needs. Staying informed about these advancements helps you anticipate future treatment options and improve your management strategies. Incorporating trailer music insights can enhance your understanding of process optimization and emotional engagement strategies across various creative fields.
Novel Biologic Agents
New biologic agents are transforming the landscape of psoriasis treatment by targeting specific immune pathways with greater precision. These emerging therapies focus on cytokines and receptors involved in the disease’s pathogenesis, offering hope for better efficacy and fewer side effects. You might see new agents targeting IL-17, IL-23, and other key molecules. They are designed to improve patient outcomes and address unmet needs in moderate-to-severe psoriasis. As these biologics evolve, they could lead to longer-lasting remission and personalized treatment plans. Keep in mind, ongoing research aims to optimize dosing, safety, and response rates. Ethical Hacking approaches are also being employed to ensure the security of digital health data associated with these innovative therapies.
Small Molecule Inhibitors
How might small molecule inhibitors shape the future of psoriasis treatment? These drugs target specific enzymes and signaling pathways involved in inflammation, offering advantages like oral administration and rapid action. You could see increased use of kinase inhibitors that interfere with key immune signals, reducing inflammation more precisely. Small molecules also tend to have shorter development times and can be less costly than biologics, making treatments more accessible. They might be combined with existing therapies to improve efficacy or used for patients who don’t respond to biologics. As research advances, you’ll likely encounter new inhibitors with improved selectivity and fewer side effects. Additionally, innovations in indoor gardening and sustainable materials could inspire the development of more eco-friendly drug delivery systems. Overall, small molecule inhibitors hold promise for expanding your options and personalizing psoriasis management in the future.
Personalized Treatment Strategies
Advances in understanding the immune pathways involved in psoriasis are paving the way for more personalized treatment strategies. Now, you can tailor therapies based on individual immune profiles, improving outcomes and reducing side effects. Emerging diagnostic tools analyze biomarkers and genetic factors to identify the most effective treatments for each patient. This approach shifts the focus from a one-size-fits-all model to precision medicine. By customizing therapies, you can target specific cytokines or immune cells driving your condition. This not only enhances effectiveness but also minimizes unnecessary medication exposure. As research progresses, expect to see more options that adapt to your unique immune response, offering better control and quality of life.
- Biomarker-based treatment selection
- Genetic profiling for personalized therapies
- Immune pathway targeting
- Monitoring response for therapy adjustments
Personalized Medicine Approaches for Psoriasis Management
Personalized medicine has emerged as a promising approach to improving psoriasis management by tailoring treatments to individual patient profiles. By analyzing genetic, immunologic, and environmental factors, you can select therapies that are more effective and have fewer side effects. This approach allows for better disease control and improved quality of life. For example, some patients respond better to biologics targeting specific immune pathways, while others benefit from topical agents or phototherapy. Here’s a quick overview:
| Patient Profile | Treatment Options | Expected Outcomes |
|---|---|---|
| Genetic markers | Biologics, small molecules | Faster clearance, fewer flare-ups |
| Immune response | Topicals, phototherapy | Symptom relief, skin healing |
| Environmental factors | Lifestyle modifications | Reduced triggers, sustained remission |
This tailored strategy empowers you to manage psoriasis more effectively.
The Importance of Ongoing Research in Immune Pathways

Ongoing research into immune pathways is vital for uncovering new targets and refining existing treatments for psoriasis. It helps you understand the disease better, leading to more effective and personalized therapies. As scientists explore immune mechanisms, they identify novel cytokines, cells, and signaling routes involved in psoriasis. This ongoing work accelerates the development of targeted drugs, improving patient outcomes.
- Identifies new biomarkers for diagnosis and disease activity
- Reveals mechanisms behind treatment resistance
- Enables development of combination therapies
- Promotes understanding of comorbidities linked to immune dysregulation
Continued research keeps you at the forefront of innovative treatments, ensuring better management and quality of life for those with psoriasis.
Frequently Asked Questions
How Does Psoriasis Affect Overall Immune System Health?
You might wonder how psoriasis impacts your overall immune health. It causes your immune system to overreact, leading to inflammation and skin cell buildup. This heightened response can sometimes weaken your immune defenses, making you more prone to infections. While your immune system is busy fighting these skin issues, it may become less effective at protecting you from other illnesses. Managing psoriasis helps restore balance and supports your immune health.
Are There Lifestyle Factors That Influence Immune Pathways in Psoriasis?
You might think lifestyle changes only affect your daily routine, but they also influence your immune pathways in psoriasis. Smoking and excessive alcohol can trigger inflammation, while a balanced diet rich in omega-3s and antioxidants can soothe immune responses. Regular exercise reduces stress and boosts immunity, helping control flare-ups. Managing weight and avoiding skin irritants also support healthier immune function, making lifestyle choices powerful allies against psoriasis.
Can Diet Changes Improve Immune Responses in Psoriasis Patients?
You might wonder if diet changes can boost immune responses in psoriasis patients. While research is still emerging, eating anti-inflammatory foods like fruits, vegetables, and omega-3 rich fish could help reduce inflammation. Avoiding processed foods, excessive sugar, and alcohol may also improve your immune function. Incorporating these dietary adjustments, along with a healthy lifestyle, can support your immune system and potentially lessen psoriasis flare-ups.
What Are the Potential Side Effects of New Immune-Targeted Therapies?
Think of new immune-targeted therapies as double-edged swords—you might gain significant relief, but risks lurk beneath the surface. You could experience side effects like infections, headaches, or skin reactions. Rarely, more serious issues like allergic responses or organ problems may occur. It’s essential to stay vigilant, communicate with your doctor, and weigh these potential dangers against the benefits of clearer skin and improved quality of life.
How Does Psoriasis Differ From Other Autoimmune Skin Conditions?
You notice psoriasis differs from other autoimmune skin conditions mainly because it involves rapid skin cell growth and inflammation, leading to thick, scaly patches. Unlike eczema, which causes itchy, inflamed skin, psoriasis often presents with well-defined plaques. Its immune response is primarily driven by T cells and cytokines like IL-17 and IL-23, making treatments targeting these pathways more effective compared to therapies for other autoimmune skin diseases.
Conclusion
Understanding the immune pathways in psoriasis reveals a complex dance of cytokines and cells, much like a finely tuned orchestra. As new therapies target these pathways, you gain hope for more effective, personalized treatments. While research uncovers deeper layers of immune dysregulation, it also offers brighter horizons. With each discovery, you’re empowered to face psoriasis with knowledge and confidence, knowing that science is actively turning the tide from uncertainty to control.









