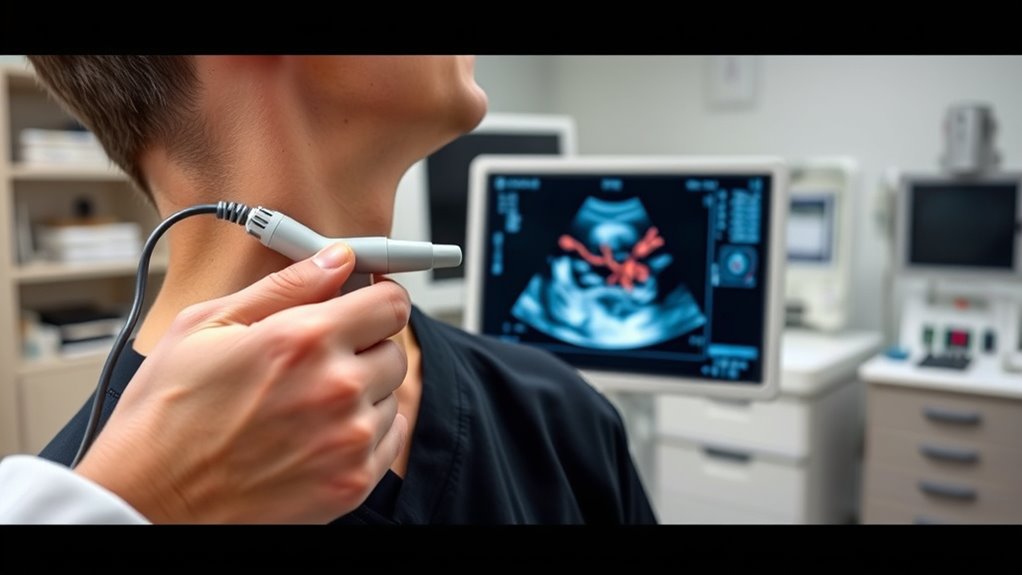
Point-of-care ultrasound (POCUS) allows you to quickly assess patients at the bedside, providing real-time images that aid in rapid diagnosis of critical conditions like cardiac, abdominal, or trauma injuries. Its portability, improved image quality, and integration with AI make it easier to acquire accurate results without waiting for traditional imaging. Mastering POCUS skills ensures effective use in emergencies and routine care. If you’re interested, you’ll discover how ongoing advancements and training can enhance your diagnostic capabilities.
Key Takeaways
- POCUS enables real-time bedside imaging for quick assessment of critical conditions like cardiac, abdominal, and trauma cases.
- Proper training and standardized protocols improve accuracy and reliability of rapid diagnoses with POCUS.
- Technological advancements, including AI integration and wireless connectivity, enhance diagnostic speed and interpretation.
- POCUS reduces time to diagnosis, minimizes patient movement, and expedites clinical decision-making in urgent scenarios.
- Widespread adoption relies on ongoing training, certification, and quality assurance to ensure safe and effective use.
The Evolution of Point-of-Care Ultrasound Technology

The evolution of point-of-care ultrasound (POCUS) technology has transformed medical practice by making imaging more accessible and immediate. Initially, ultrasound devices were bulky, expensive, and confined to specialized imaging labs. Over time, advancements led to portable, handheld units that fit in your pocket, allowing you to perform scans right at the patient’s bedside. Improvements in battery life, image resolution, and user interface made POCUS more practical for diverse clinical settings. Today, you can quickly obtain real-time images, aiding in faster diagnoses and decision-making. These technological leaps have shifted ultrasound from a resource-heavy tool to an everyday clinical instrument, empowering you to assess, monitor, and diagnose patients swiftly, often reducing the need for more invasive or time-consuming procedures. Cost-effective strategies have also played a role in making POCUS more widely adopted across healthcare settings.
Essential Skills for POCUS Application

Mastering probe handling techniques guarantees you get accurate images quickly and comfortably. You also need to cultivate image optimization skills to enhance clarity and diagnostic value. Together, these core abilities form the foundation for effective POCUS application. Incorporating knowledge of security features can help ensure the safety of your equipment and environment during procedures.
Probe Handling Techniques
Effective probe handling is fundamental to obtaining clear, diagnostic-quality images during point-of-care ultrasound. You should hold the probe firmly but comfortably, avoiding excessive pressure that could distort anatomy. Use your non-dominant hand to stabilize the probe, keeping it steady while you’re scanning. Position the probe with gentle, deliberate movements to maintain consistent contact with the skin. Adjust your grip as needed to improve maneuverability, especially when changing angles or depths. Keep your fingers close to the probe to facilitate quick adjustments. Maintain a relaxed wrist to reduce fatigue and improve control. Consistent, smooth movements help produce steady images, minimizing artifacts. Proper probe handling ensures you capture accurate visuals quickly, which is critical for effective rapid diagnosis in urgent clinical settings. Additionally, understanding how exfoliation impacts skin clarity can help optimize ultrasound gel application for better contact and image quality.
Image Optimization Skills
Once you’ve established proper probe handling, fine-tuning your image quality becomes the next key step. You can improve clarity by adjusting your depth to focus on the area of interest, ensuring the target structures fill the screen appropriately. Use the gain control to optimize brightness—neither too dark nor too bright—so details are visible without distortion. Pay attention to focus settings; positioning the focal zone at or just below the structure enhances resolution. Slightly angling or rocking the probe can reduce artifacts and improve image clarity. Consistently adjusting these settings during your scan helps you obtain the clearest, most diagnostic image possible. Mastering these optimization skills ensures rapid, accurate assessments in critical situations. Additionally, familiarizing yourself with different headphone jacks can be beneficial when connecting audio components or troubleshooting device compatibility issues.
Common Clinical Uses of POCUS in Emergency Medicine

You’ll find POCUS invaluable for quickly evaluating cardiac function and identifying life-threatening issues. It also allows you to evaluate abdominal emergencies efficiently at the bedside. These applications help you make faster, more informed decisions in critical situations. For example, understanding performance tuning techniques can enhance your interpretation of ultrasound findings by recognizing signs of improved or compromised organ function.
Cardiac Function Assessment
Evaluating cardiac function is a crucial application of point-of-care ultrasound (POCUS) in emergency medicine, especially when rapid decisions are necessary. You can quickly assess ventricular size and contractility to identify heart failure or cardiogenic shock. Using the parasternal long-axis and apical views, you evaluate the left ventricle’s systolic function, noting hypokinesis or reduced ejection fraction. You also examine the right ventricle for dilation, which can indicate pulmonary embolism or right-sided failure. Additionally, you look for pericardial effusion that might cause tamponade. POCUS allows you to detect gross abnormalities in cardiac motion and chamber size, guiding immediate management. Notably, emerging sneaker technologies are being integrated into medical equipment to enhance imaging capabilities and portability. This real-time assessment helps you determine the urgency of interventions and decide whether advanced imaging or cardiology consultation is necessary.
Abdominal Emergency Evaluation
Point-of-care ultrasound (POCUS) plays a vital role in rapidly evaluating abdominal emergencies in the emergency department. It allows you to quickly identify life-threatening conditions, guiding immediate management. With POCUS, you can assess for free fluid in the abdomen, which suggests internal bleeding, or detect signs of appendicitis, such as a non-compressible, enlarged appendix. It also helps identify gallstones or biliary obstruction in suspected cholecystitis. Effective detection methods enhance diagnostic accuracy and patient outcomes.
Key applications include:
- Detecting free fluid in trauma or ruptures
- Identifying appendicitis or other causes of acute abdomen
- Evaluating gallbladder pathology
Using POCUS streamlines diagnosis, reduces time to treatment, and minimizes reliance on more invasive or time-consuming imaging techniques.
Advantages of Rapid Bedside Diagnosis

Rapid bedside diagnosis with point-of-care ultrasound allows healthcare providers to quickly identify critical conditions, often before laboratory results are available. This immediacy enables you to make faster decisions, prioritize care, and initiate appropriate treatments without delay. It reduces the need for multiple tests, saving time and resources, while minimizing patient movement and exposure. You gain real-time insights into anatomy and pathology, improving diagnostic accuracy in emergency situations. This rapid assessment can be lifesaving, especially in unstable patients where every second counts. Additionally, bedside ultrasound enhances your confidence in clinical decision-making by providing visual confirmation of suspected diagnoses. Incorporating high-quality ultrasound equipment with excellent image clarity further improves diagnostic precision. Overall, it streamlines workflows and improves patient outcomes through swift, accurate, and non-invasive evaluation.
Integrating POCUS Into Routine Practice
To effectively incorporate POCUS into routine practice, healthcare providers must develop structured protocols and guarantee consistent training. This ensures reliable, accurate results and smooth integration into patient care. Clear protocols help define when and how to use ultrasound, reducing variability. Ongoing training maintains skill levels and keeps you updated on new techniques. To successfully embed POCUS, consider these key steps: Establish standardized procedures and checklists — dream journaling can help reinforce skills and improve recall of findings. Implement regular training sessions and skills assessments. Incorporate POCUS into daily workflows and clinical decision-making
Challenges and Limitations of POCUS

While POCUS offers numerous advantages, it also presents several challenges that healthcare providers must navigate. One major limitation is operator dependency; your skill and experience directly impact image quality and diagnostic accuracy. Inconsistent training can lead to misinterpretation, affecting patient outcomes. Equipment limitations also pose hurdles—portable devices may lack the resolution needed for detailed assessments. Additionally, POCUS has limited penetration depth and field of view, making it less effective for certain patients or conditions. Time constraints in emergency settings can hinder exhaustive examinations, and over-reliance on ultrasound might lead to missed diagnoses if used without corroborating tests. Finally, cost and maintenance of devices can be barriers, especially in resource-limited settings. Recognizing these challenges helps you optimize POCUS use and improve patient care. Sound healing science emphasizes the importance of understanding the tools and techniques used in diagnostic processes.
Case Studies Highlighting POCUS Effectiveness

Case studies clearly demonstrate how point-of-care ultrasound can substantially improve patient outcomes in diverse clinical scenarios. For example, in emergency departments, POCUS rapidly identified aortic dissections, enabling immediate surgical intervention. In rural settings, it helped diagnose pneumonia, reducing unnecessary antibiotic use and hospital transfers. Additionally, in trauma cases, bedside ultrasound detected internal bleeding, guiding swift decisions and saving lives. These cases highlight POCUS’s ability to:
- Accelerate diagnosis in critical situations
- Reduce reliance on time-consuming imaging
- Improve accuracy in resource-limited environments
Future Developments in Portable Ultrasound Devices

Advancements in portable ultrasound technology are poised to transform point-of-care imaging further, making devices smaller, more affordable, and easier to use across diverse clinical settings. Future devices will integrate artificial intelligence for real-time image analysis, helping you interpret findings quickly. Enhanced battery life and wireless connectivity will allow seamless data sharing, improving patient care. Expect innovations like flexible, foldable probes and improved image resolution, increasing versatility. As a result, you’ll find it easier to perform exams in remote locations or crowded emergency rooms. These developments will streamline workflows, reduce costs, and expand access to quality diagnostics.
| Feature | Benefit | Impact |
|---|---|---|
| AI-powered analysis | Faster diagnosis | Improved clinical decision-making |
| Wireless data transfer | Enhanced connectivity | Better collaboration |
| Flexible, foldable probes | Greater maneuverability | Broader application scope |
| Longer battery life | Increased portability | Extended use in field settings |
| High-resolution imaging | Clearer, more accurate images | Improved diagnostic confidence |
Training and Certification for POCUS Practitioners

Effective training and certification are essential to guarantee that you can perform point-of-care ultrasound (POCUS) safely and accurately. Proper education ensures you develop the necessary skills to interpret images correctly and make confident clinical decisions. Certification programs validate your proficiency and demonstrate your commitment to quality care. To succeed, focus on:
- Participating in accredited courses that combine hands-on practice with theoretical knowledge
- Gaining supervised clinical experience to build confidence and competence
- Staying current with ongoing education and recertification requirements to maintain your skills
Frequently Asked Questions
How Does POCUS Compare to Traditional Imaging Methods?
You’ll find that POCUS offers rapid, bedside assessment, making it more immediate than traditional imaging like CT or MRI, which often require scheduling and transport. It’s portable, easy to use, and provides real-time results, helping you make quicker decisions. However, it may be less detailed than exhaustive imaging. So, while POCUS enhances speed and convenience, traditional methods still excel in detailed, high-resolution images when extensive analysis is needed.
What Are the Cost Implications of Implementing POCUS?
When considering the cost implications of implementing POCUS, you’ll find it can be quite cost-effective. It reduces the need for expensive, time-consuming traditional imaging like CT or MRI, leading to lower overall expenses. Plus, it allows for quicker diagnoses, which can decrease hospital stays and improve patient outcomes. Although initial training and equipment costs exist, the savings and efficiency gains often outweigh these, making POCUS a financially smart choice.
How Can POCUS Be Used in Resource-Limited Settings?
You can use POCUS in resource-limited settings to improve diagnosis and patient outcomes without relying on expensive, centralized imaging facilities. It’s portable, affordable, and provides immediate results, making it ideal where access to traditional imaging is limited. You can quickly assess conditions like fluid in the lungs, abdominal issues, or pregnancy complications, helping you make rapid decisions and deliver timely care despite resource constraints.
What Are Common Pitfalls in POCUS Interpretation?
When interpreting POCUS, you should be aware of common pitfalls like misidentifying normal structures as abnormal, over-relying on a single image, and neglecting clinical context. Make certain you verify findings with multiple views, consider patient history, and avoid rushing the interpretation. Remember, artifacts can mimic pathology, so stay cautious. Continuous practice and correlation with other diagnostic tools help improve accuracy and reduce misinterpretation risks.
How Is POCUS Integrated Into Interdisciplinary Patient Care?
They say, “Teamwork makes the dream work,” and in interdisciplinary patient care, you play a vital role. You integrate POCUS by collaborating with physicians, nurses, and specialists, providing real-time insights that guide decisions. You communicate findings clearly, ensuring everyone’s on the same page. This seamless integration helps expedite diagnoses, tailor treatments, and improve outcomes, emphasizing that effective teamwork and timely information are key to delivering essential patient care.
Conclusion
Embrace point-of-care ultrasound as your guiding light in urgent moments, symbolizing clarity amid chaos. Like a lighthouse piercing through fog, POCUS transforms uncertainty into understanding, empowering you to make swift, confident decisions. As technology advances, it becomes your steadfast companion on the journey of bedside diagnosis. Remember, mastering this tool isn’t just about skills—it’s about illuminating the unseen, turning shadows of doubt into the bright horizon of informed care.









